Burden of insulin resistance

Resistance to insulin has been linked to many major diseases in humans. This includes diabetes, obesity, polycystic ovarian syndrome and metabolic syndrome. These diseases have reached epidemic levels in recent years. Finding ways to reverse the biologic processes that drive insulin resistance can help lead to new treatments for these conditions.
Relationship between insulin sensitivity and insulin secretion
There is an established inverse relationship between insulin sensitivity and insulin secretion. This demonstrates a redundant mechanism to face glucose homeostasis in the setting of metabolic perturbations that lead to insulin resistance. Recent evidence suggests that progression to type 2 diabetes results not only from insulin decreased insulin sensitivity (insulin resistance) but also from loss of insulin secretion. Patients with severe insulin resistance exist a the top upper left hand corner of this chart. This is interesting as they possess a unique ability to secrete extremely high degrees of insulin resistance.

Insulin and growth
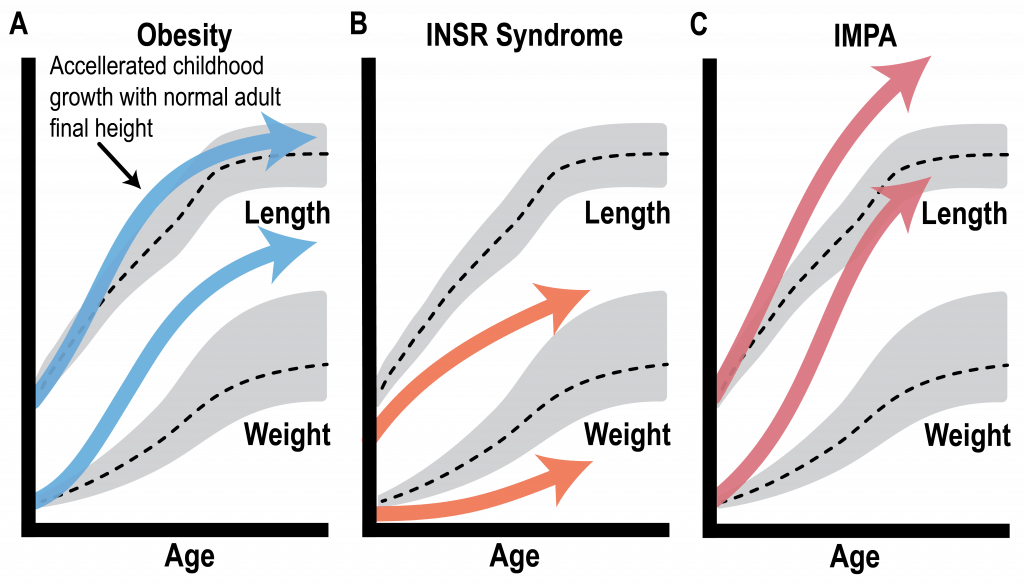
Beyond its role in regulating blood glucose, insulin plays an important role as a growth factor. Interestingly, children with obesity experience transient linear growth accelerations. However, children with insulin receptor (INSR) mutations experience failure to thrive. While extensive efforts have studied insulin receptor defects, severe insulin resistance syndromes downstream of the insulin receptor have been understudied. Interestingly, patients with downstream defects of insulin signaling experience overgrowth and tall stature. Potentially via excess insulin activating growth promoting pathways. This phenomena, pseudoacromegaly appears clinically like growth hormone excess, with normal growth hormone levels.
Insulin-mediated pseudoacromegaly (IMPA)
Insulin mediated pseudoacromegaly (IMPA) is an extremely rare disorder of insulin resistance. Patients affected with this condition have high blood sugar, obesity and very tall stature. Women with this disease often have excessive body hair and irregular menstrual cycles. Patient with IMPA have physical signs of growth hormone excess (gigantism or acromegaly), however their growth hormone levels are normal. However, patients with IMPA have extremely high insulin levels. Therefore, IMPA is classified as an insulin resistance syndrome. Thus far there is no known genetic or molecular cause of this disease, however, our research group was the first to publish a possible genetic cause of this disease.
Possible genetic causes of IMPA
Whole exome sequencing, performed on a proband with IMPA, her younger sibling, and parents, identified deleterious variants in genes critical to the Fibroblast Growth Factor 21 (FGF21) signaling pathway (FGFR1 and KLB) in both the proband and her younger sibling. Interestingly, the younger sibling is showing early-stage phenotypes that resemble the proband. FGFR1 (FGF Receptor 1) and KLB (β-klotho) form a transmembrane receptor- cofactor complex that binds FGF21.
Fibroblast growth factor 21 (FGF21)
The FGF family is composed of both canonical FGFs and endocrine FGFs. Canonical FGFs require heparan/heparan sulfate as a cofactor and act in an autocrine or paracrine fashion. While the endocrine FGFs (including FGF21 and FGF23) use a transmembrane protein cofactor (alpha or beta-klotho) to exert their effects on distant tissues. FGF21 is a hepatokine which is regulated by PPARα acts to regulate the body’s response to starvation through CNS and peripheral target tissues. Increased levels of FGF21 are associated with obesity, fatty liver and atherogenic lipid profiles. This suggests that metabolic syndrome is an FGF21 resistant state.
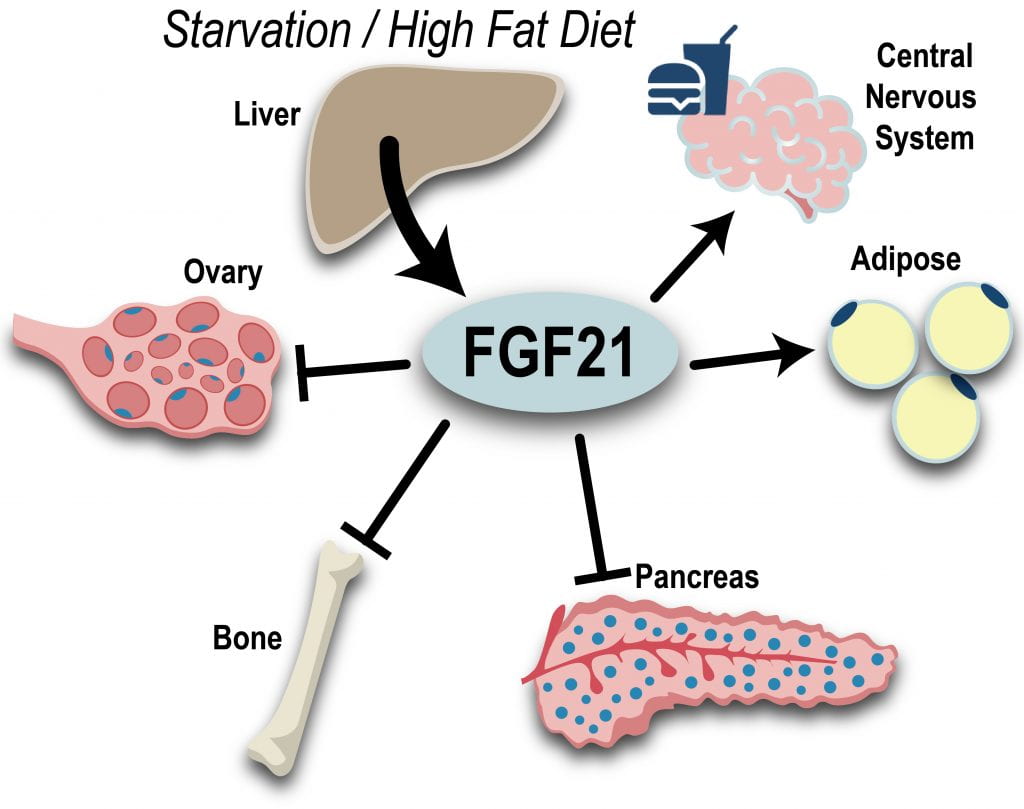
Therefore, resistance to FGF21 could explain the insulin resistance, hyperinsulinemia, obesity and overgrowth seen in IMPA. Our lab is actively pursuing this area of research.
Learn more about known types of severe insulin resistance.